Image Wisely, a joint initiative of ACR, RSNA, ASRT and AAPM,
provides information to the medical community to promote safety in medical imaging.

Team Performance
James Duncan, MD, PhD, Mallinckrodt Institute of Radiology, St. Louis, MO
Download PDF

Teamwork is an essential part of fluoroscopic procedures. No single individual can be expected to understand every detail of the fluoroscope’s operation, possess all the knowledge needed to effectively use it during fluoroscopic procedures or provide continuous 24/7 coverage over an extended period. As a result, radiation safety during fluoroscopic procedures depends on an extensive network of people working together as a team.
| Team Members | Typical Responsibilities | Typical Role | ||
| Primary Operator (physician or midlevel) | Control the fluoroscope. Obtain and interpret diagnostic images. Perform the desired intervention. Monitor radiation use. | Primary | ||
| Technologist | Select and adjust imaging protocols. Assist with patient positioning. Monitor radiation use and provide alerts at predetermined thresholds. Archive images and dose reports. Perform quality assurance tasks. | Primary | ||
| Nurse, Anesthesiologist | Monitor patient condition, administer medications, ensure patient comfort | Primary | ||
| Patient | Follow instructions and provide feedback on team performance | Primary | ||
| Medical Physicist | Monitor equipment, analyze radiation use, design imaging protocols | Support | ||
| Service Engineer | Service equipment and install imaging protocols | Support | ||
| Vendor | Design and produce imaging equipment and disposable supplies | Support | ||
| Reception, Scheduling, Coordinators | Receive requests, schedule procedures, coordinate follow-up | Support | ||
| Administration, Housekeeping | Design and service the working environment | Support | ||
| Quality/Safety Officers | Review reports of radiation use, coordinate event investigations, interact with oversight agencies | Support | ||
| Referring Physician | Request procedures, act on results | Support |
Factors Influencing Individual Performance
The performance of any system ultimately depends on the expertise of the personnel who design and operate it [1]. Experts are highly valued because when all other factors are equal, experts provide the best chance of achieving the desired result. However, the linkage between expertise and superior results can be broken by factors such as sleep deprivation, poor teamwork, uncooperative patients, production pressure, faulty fluoroscopes, environmental distractions or inadequate supplies [2].
While some might contend that expertise is innate and skills such as hand-eye coordination are hardwired, analysis of expert performance in a wide variety of fields finds that mastery requires 10 years and 10,000 hours of practice with feedback [3]. Experience by itself does not lead to improved performance; rather it must be matched with feedback, particularly analysis of errors.
For radiation safety during fluoroscopic procedures, it should not be surprising that novices routinely make errors such as keeping their foot on the pedal while not looking at the monitor, activating the fluoroscope before centering over the field of interest or collecting more images than necessary to answer the question at hand. Practice with feedback allows one to develop and refine safe habits. Practice with feedback also expands one’s library of visual patterns associated with clinical conditions and interventional tasks.
Fundamentals of Teamwork
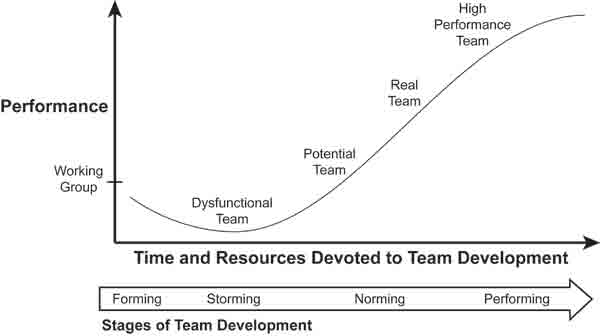
Teamwork requires coordinated execution of individual actions. For radiation safety during fluoroscopic procedures, high performing teams greatly exceed the capabilities of individuals, no matter their skill, intelligence or dedication. Individual members of the team share their understanding of the situation at hand. The resulting shared mental models describe the actions needed to optimize performance for each segment of the overall procedure [4]. While team members are often able to observe each other’s actions, the plans or mental models that underlie those actions are not observable. Sharing mental models and resolving any conflicts or ambiguities between team members requires communication and trust. As a result, developing high performing teams is difficult and requires time (Figure 1) [5].
Figure 1: Stages of team development
How Teamwork Improves Radiation Safety During Fluoroscopic Procedures
Technologists monitoring cumulative radiation metrics during complex procedures
Complex procedures often require focused problem solving by the primary operator. The resulting “tunnel vision” causes attention to focus on task planning and execution. As a result, the primary operator may have little or no mental bandwidth available to monitor cumulative radiation exposure. In such situations, technologists and other team members can step in and provide gentle reminders when thresholds such as 3 Gy reference point air kerma or 30 minutes of fluoroscopy time are reached.
Monitoring vital signs and the level of sedation during procedures
Many interventional procedures are performed with sedation. Ideally patients are not uncomfortable during their procedures and still able to follow commands such as suspending respiration or holding still to minimize subtraction artifacts during DSA runs. Achieving this balance requires not only monitoring the patient but also benefits from a shared mental model of which procedure segments require cooperation versus those that can cause pain. Repeating a DSA run due to motion artifact, or even worse missing a key finding, increases the harm and lowers the benefit respectively of fluoroscopic procedures.
Medical physicists and service engineers working with clinical teams to create low-dose protocols and use them as the default setting
Sequences of fluoroscopic images provide dynamic feedback of the procedure’s progress. Frame rates and other settings are often adjusted to match the information flow needed to complete the task. Undersampling provides an insufficient flow of information and this is clearly evident to the operator. The typical response is to adjust settings until information flow matches the procedure’s needs. In contrast, oversampling provides redundant information and there is no immediate impetus to revise settings. Stated another way, while it is common to see clinical teams shift from low dose to higher dose protocols during complex segments of a procedure, it is rare to see them shift back to the low dose protocols once the difficult segment is completed. This highlights the need to create low dose protocols and use them as the default setting for starting procedures. A recent analysis found that such a process led to a sustained 50% reduction in average dose/procedure [6].
References
- Reason JT. Managing the risks of organizational accidents. Aldershot, Hants, England; Brookfield, VT, USA: Ashgate; 1997. Available at: http://books.google.com/books?id=ZnhRAAAAMAAJ&q. Accessed September 24, 2014.
- Bucholz EI, Duncan JR. Assessing system performance. JVIR, 2008. 19(7):987-994. Available at: http://www.jvir.org/article/S1051-0443(08)00292-3/fulltext. Accessed October 16, 2014.
- Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Academic medicine: Journal of the Association of American Medical Colleges, 2004. 79(10 Suppl):S70-81. Available at: http://journals.lww.com/academicmedicine/Fulltext/2004/10001/Deliberate_Practice_and_the_Acquisition_and.22.aspx/. Accessed October 16, 2014.
- Senge PM. The fifth discipline: the art and practice of the learning organization. Rev. and updated. ed. New York: Doubleday/Currency; 2006. Available at: http://books.google.com/books?id=b0XHUvs_iBkC&dq. Accessed September 24, 2014.
- Tuckman BW. Developmental sequence in small groups. Psychological Bulletin, 1965. 63:384-399. Available at: http://www.ncbi.nlm.nih.gov/pubmed/14314073. Accessed September 24, 2014.
- Duncan JR, Street M, Strother M, Picus D. Optimizing radiation use during fluoroscopic procedures: a quality and safety improvement project. J Am Coll Radiol. Nov 2013;10(11):847-853. Available at: http://www.jacr.org/article/S1546-1440(13)00281-0/fulltext. Accessed October 16, 2014.



