Image Wisely, a joint initiative of ACR, RSNA, ASRT and AAPM,
provides information to the medical community to promote safety in medical imaging.

Factors Influencing Radiation Use During Fluoroscopic Procedures
James Duncan, MD, PhD, Mallinckrodt Institute of Radiology, St. Louis, MO
Published November 25, 2014 | Download PDF

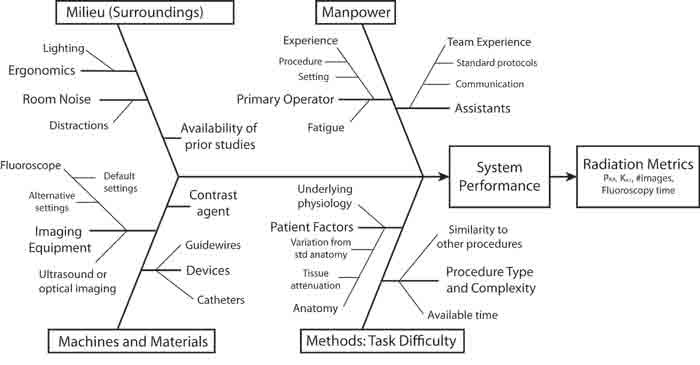
The factors governing system performance are often divided using a “6 M” approach (Machines, Manpower, Materials, Measurements, Milieu, Methods). Figure 1 illustrates how these broad categories can be used to begin cataloguing the numerous factors that govern radiation use during fluoroscopic procedures.
Figure 1: Factors impacting radiation use in fluoroscopy
Methods: Task Difficulty
Simple tasks are characterized by fewer intraprocedural decisions and this in turn leads to acquiring fewer images [1,2]. For a simple procedure such as ultrasound-guided central venous catheter placement, the question of whether the guidewire passed into the central veins can often be answered with a single fluoroscopic image.
In the same manner, the final position of the catheter tip can also be assessed with a single image. In procedures where fluoroscopy rather than ultrasound is used to help guide the needle to a target point, additional images might be needed to help select the starting point on the overlying skin and monitor the needle tip as it is advanced to the target’s location.
In contrast, more complex tasks such as IVC filter placement include more intraprocedural decisions and more images are typically needed to inform these decisions. In addition to confirming that the guidewire passes into the IVC, images are typically used to monitor the position of the flush catheter. Another series of DSA images are used to assess IVC anatomy and determine the desired location for filter deployment. A subsequent series of fluoroscopic images are used to assess positioning of the sheathed IVC filter prior to its deployment. Additional images are used to monitor its position during deployment and confirm complete deployment.
For retrievable filters, additional images are often acquired during contrast injection to assess for filter tilting or other issues that might complicate future retrieval. Indeed, tilted filters have often been immediately recovered and redeployed, which is accompanied by the acquisition of even more images.
Task difficulty clearly depends on the complexity of the desired procedure as well as the patient’s underlying anatomy and physiology. While procedures are typically described in general terms such as biliary drainage or pelvic embolization, such general descriptions confound analytic efforts because they are not well standardized.
Billing codes offer a more detailed and standardized set of descriptions. Procedures such as central venous catheter placements are described using a string of CPT® codes where each term in the string provides insights into how the procedure was performed. Using several CPT codes to describe procedures is analogous to using short messages and a limited vocabulary to describe complex circumstances [3].
As a result, key information is clearly lost during this translation. Although one frequently gathers additional information from the dictated report, the key details of the patient’s anatomy and physiology that warranted variations from the procedure’s standard sequence are almost never described in sufficient detail to recreate all the factors that altered the procedure’s difficulty.
Another useful means of assessing task difficulty is time devoted to making intraprocedural decisions [4]. Thus while fluoroscopy time is a poor surrogate for radiation use, it provides an estimate of the number and complexity of intraprocedural decisions. Indeed, cognitive psychologists derived the Hick-Hyman rule as a means of expressing the strong relationship between decision time and task difficulty. For example, a more complex than normal IVC filter placement may still be described using CPT 37191, but the additional complexity will be signaled by a longer than normal fluoroscopy time.
Manpower
The combined and coordinated skills of the primary operator and assistants can have a dramatic impact on system performance. Highly skilled teams make short work of complex tasks. In contrast, less skilled teams can spend minutes to hours struggling with simple tasks. While system performance clearly depends on the skill of the primary operator, almost all procedures require the coordinated efforts of technologists and nurses. Coordination depends on communication and shared mental models, both of which are improved via prior experience working together. Unfortunately, fatigue and other human frailties can negate years of such experience and markedly degrade overall performance.
Machines and Materials
The team’s performance also depends on the capabilities of the available tools. Performance dramatically declines if key tools are unavailable and not functioning properly. The latter occurs when imaging equipment is not properly serviced or less than optimal imaging protocols are used. Prior imaging is a powerful tool. Preexisting information allows one to plan procedures, anticipate difficulties and develop contingencies before starting the procedure rather than during it.
Milieu
Finally, the impact of the working environment is frequently neglected. Having monitors appropriately positioned and free of glare from extraneous light sources improves performance. The deleterious impact of distractions has been well studied in other settings and there is every reason to believe that divided attention will negatively impact performance during fluoroscopic procedures.
References
- Beta E, Parikh AS, Street M, Duncan JR. Capture and analysis of data from image-guided procedures. J Vasc Interv Radiol. Jun 2009;20(6):769-781. Available at: http://www.jvir.org/article/S1051-0443(09)00221-8/fulltext. Accessed October 1, 2014.
- Duncan JR, Currie S. Assessing Physician Performance (Chapter 19). In: Abujudeh H, Bruno MA, eds. Quality and Safety in Radiology: Oxford University Press; 2012. Available at: http://global.oup.com/academic/product/quality-and-safety-in-radiology-9780199735754;jsessionid=5B7A0A1CDB31A99791F306EC9129F9D5?cc=us&lang=en&#.Accessed October 1, 2014.
- Pierce JR. An introduction to information theory: symbols, signals & noise. 2nd, rev. ed. New York: Dover Publications; 1980. Available at: http://books.google.com/books/about/An_Introduction_to_Information_Theory.html?id=fXxde44_0zsC. Accessed October 1, 2014.
- Hick WE. On the rate of gain of information. Quarterly Journal of Experimental Psychology; 1952;4(1):11-26. Available at: http://www.tandfonline.com/doi/abs/10.1080/17470215208416600#.VCwmRmTD-70. Accessed October 1, 2014.



